Do I Qualify to Become a Member of Provider Partners Health PlanS?
To learn if you (or your loved one) are likely to qualify for the services offered by Provider Partners Health Plans, please answer the following questions. Our staff also is happy to help you determine your eligibility. Just contact our Member Services number at 1-800-405-9681 for additional information. (TTY users should call 711). Hours are 8:00 A.M. to 8:00 P.M., seven days a week from October 1 through March 31; 8:00 A.M. to 8:00 P.M. Monday to Friday from April 1 through September 30.
- Do you currently have Medicare Part A (hospital insurance) and Part B (medical insurance)?
- Have you been a resident of a nursing home or skilled nursing facility for longer than ninety (90) days?
- Do you live at home and the state that you reside in has certified that you need the type of care that is usually provided in a nursing home?


Who’s eligible?
You are eligible for membership in our plan as long as:
- Must be entitled to Medicare Part A to be enrolled in Medicare Part B
- You live in one of our network nursing homes OR you live in the state of Illinois, Maryland, Missouri, North Carolina, Pennsylvania, or Texas and they have certified you need the type of care that is usually provided in a nursing home.
- You live in one of our service areas:
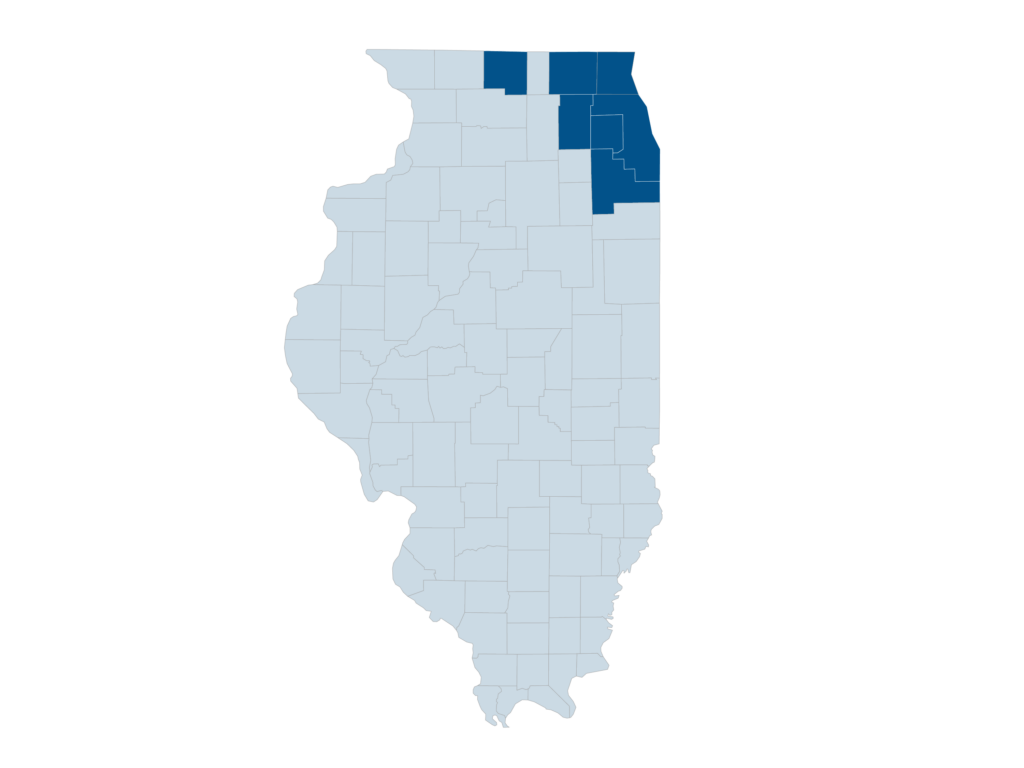
- In Illinois, Provider Partners Health Plans covers care in 7 Illinois counties – Cook, DuPage, Kane, Lake, McHenry, Will, and Winnebago.
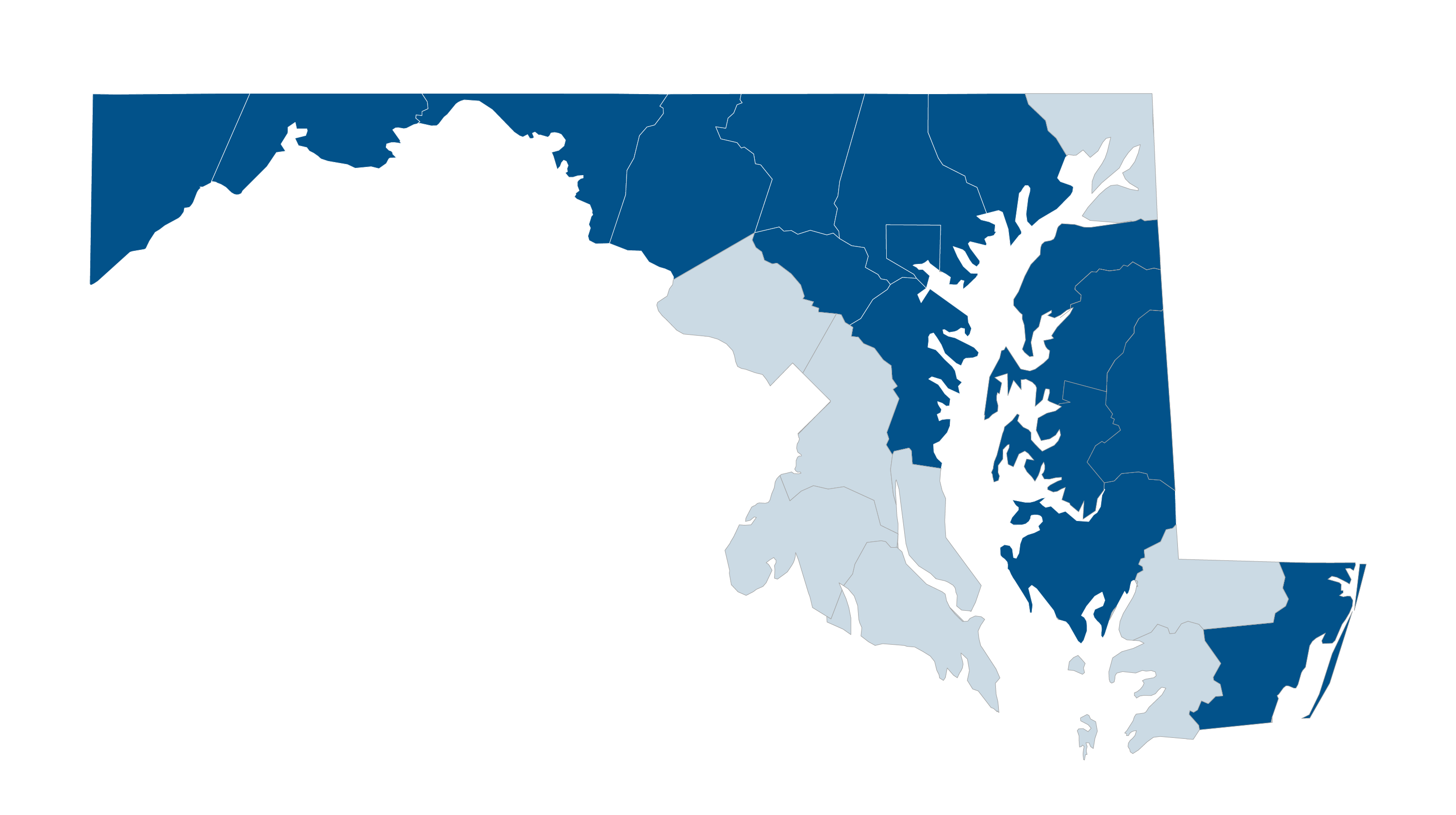
- In Maryland, Provider Partners Health Plans covers care in 16 Maryland counties – Allegany, Anne Arundel, Baltimore, Baltimore City, Caroline, Carroll, Dorchester, Frederick, Garrett, Harford, Howard, Kent, Queen Anne’s, Talbot, Washington, and Worcester.
- In Illinois, Provider Partners Health Plans covers care in 7 Illinois counties – Cook, DuPage, Kane, Lake, McHenry, Will, and Winnebago.
-
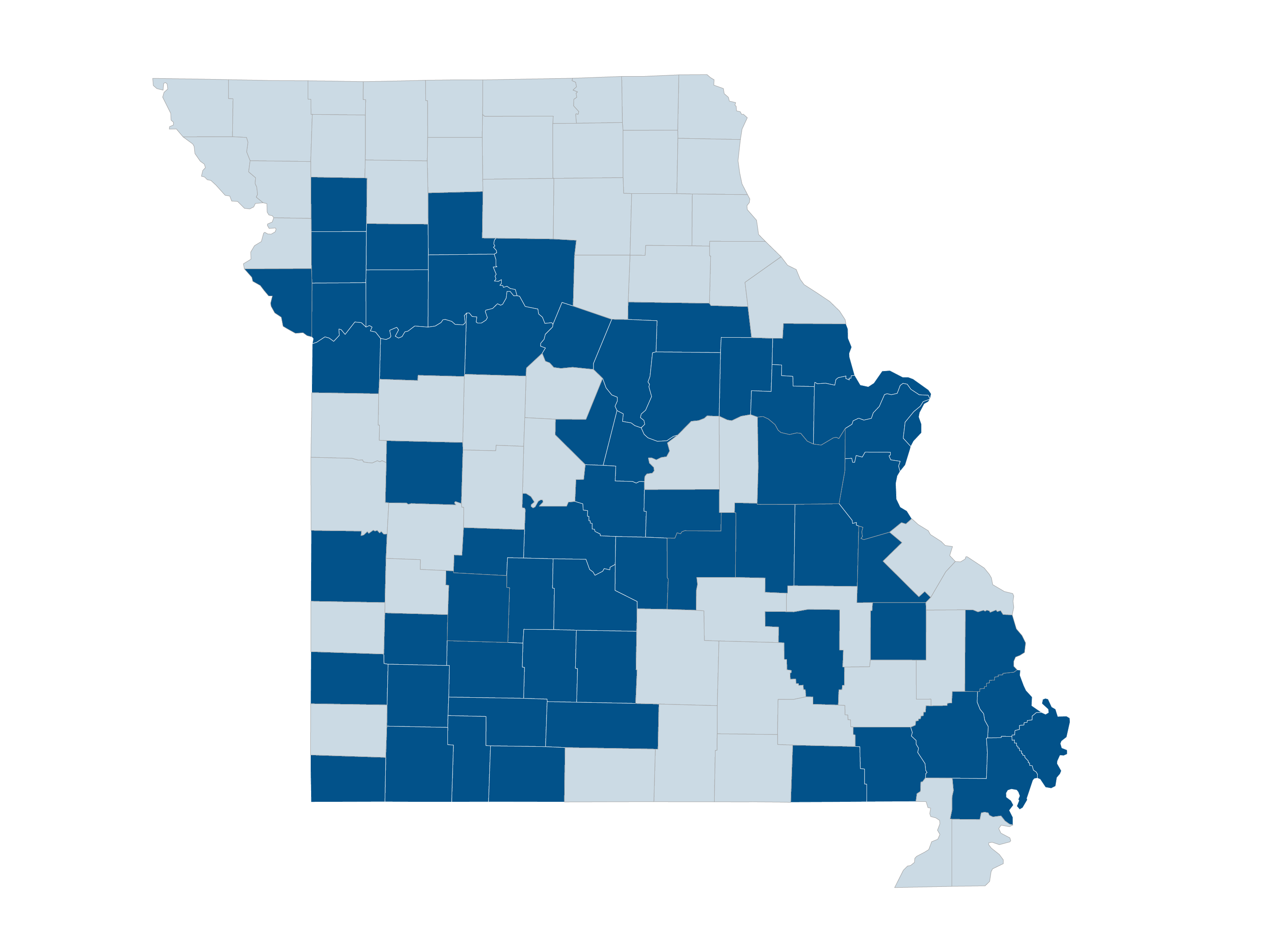
 In Missouri, Provider Partners Health Plans covers care in 61 Missouri counties – Audrain, Barry, Boone, Butler, Caldwell, Callaway, Camden, Cape Girardeau, Carroll, Chariton, Christian, Clay, Clinton, Cole, Crawford, Dade, Dallas, DeKalb, Douglas, Franklin, Greene, Henry, Hickory, Howard, Jackson, Jasper, Jefferson, Laclede, Lafayette, Lawrence, Lincoln, Livingston, Madison, Maries, McDonald, Miller, Mississippi, Moniteau, Montgomery, New Madrid, Phelps, Platte, Polk, Pulaski, Ray, Reynolds, Ripley, St. Charles, St. Francois, St. Louis, St. Louis City, Saline, Scott, Stoddard, Stone, Taney, Vernon, Warren, Washington, Webster and Wright.
In Missouri, Provider Partners Health Plans covers care in 61 Missouri counties – Audrain, Barry, Boone, Butler, Caldwell, Callaway, Camden, Cape Girardeau, Carroll, Chariton, Christian, Clay, Clinton, Cole, Crawford, Dade, Dallas, DeKalb, Douglas, Franklin, Greene, Henry, Hickory, Howard, Jackson, Jasper, Jefferson, Laclede, Lafayette, Lawrence, Lincoln, Livingston, Madison, Maries, McDonald, Miller, Mississippi, Moniteau, Montgomery, New Madrid, Phelps, Platte, Polk, Pulaski, Ray, Reynolds, Ripley, St. Charles, St. Francois, St. Louis, St. Louis City, Saline, Scott, Stoddard, Stone, Taney, Vernon, Warren, Washington, Webster and Wright.
-
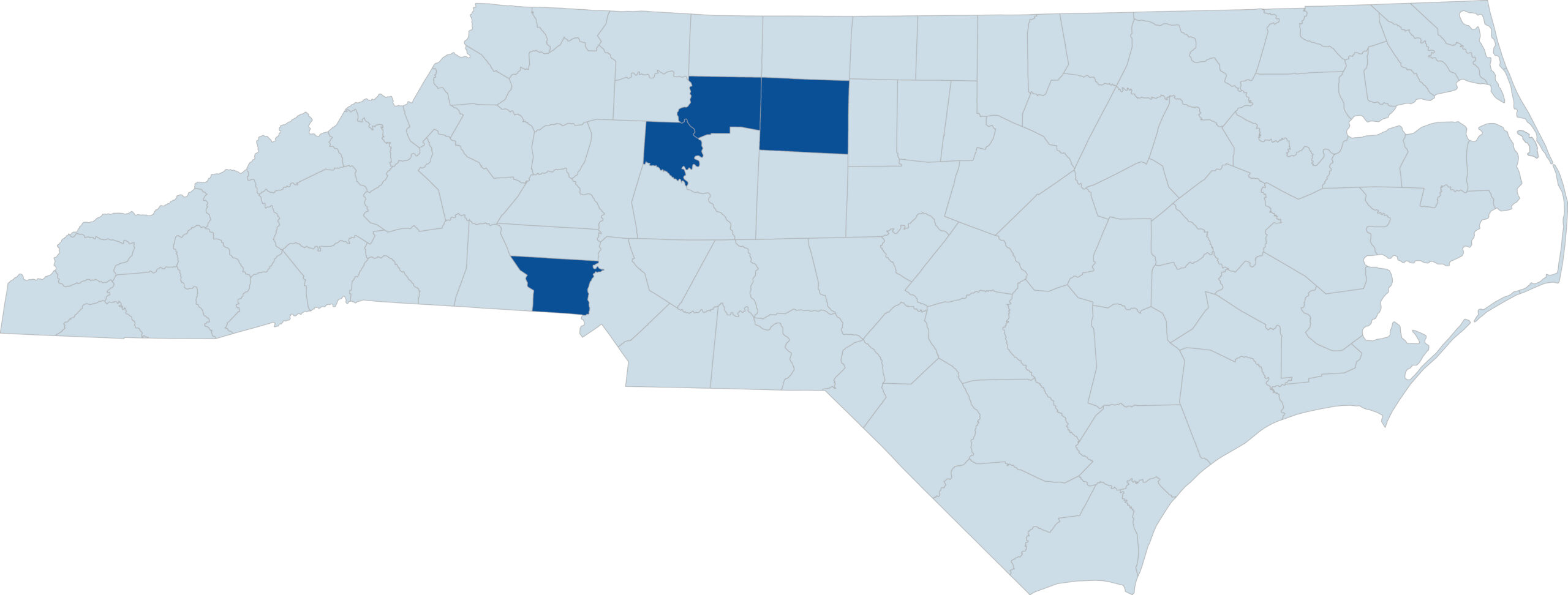
- In North Carolina, Provider Partners Health Plans covers care in 4 North Carolina counties – Davie, Forsyth, Gaston, and Guilford.
-
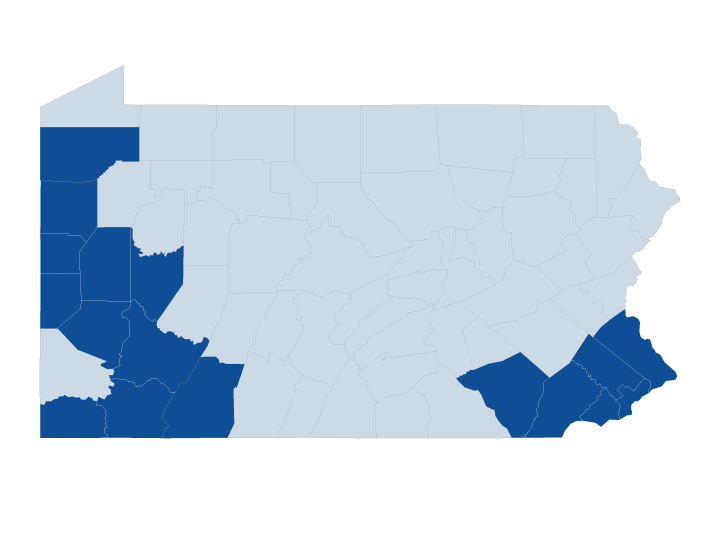
 In Pennsylvania, Provider Partners Health Plans covers care in 17 Pennsylvania counties – Allegheny, Armstrong, Beaver, Bucks, Butler, Chester, Crawford, Delaware, Fayette, Greene, Lancaster, Lawrence, Mercer, Montgomery, Philadelphia, Somerset, and Westmoreland.
In Pennsylvania, Provider Partners Health Plans covers care in 17 Pennsylvania counties – Allegheny, Armstrong, Beaver, Bucks, Butler, Chester, Crawford, Delaware, Fayette, Greene, Lancaster, Lawrence, Mercer, Montgomery, Philadelphia, Somerset, and Westmoreland.
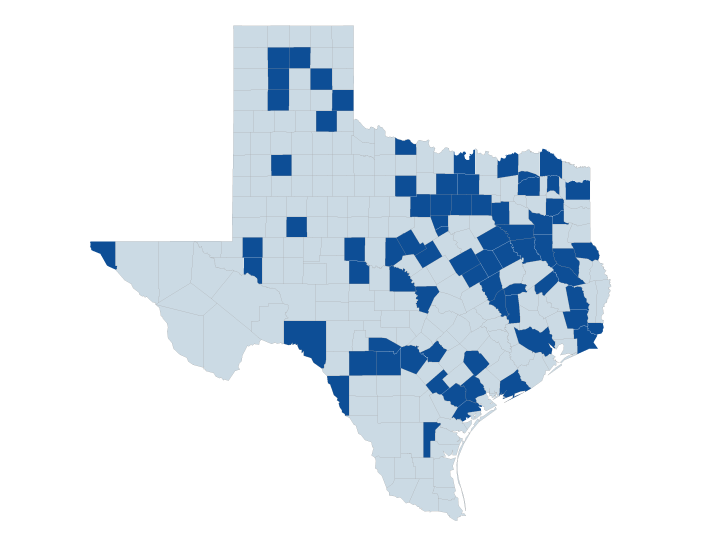
- In Texas, Provider Partners Health Plans covers care in 76 Texas counties – Anderson, Angelina, Bandera, Bexar, Brazos, Brown, Burnet, Cass, Cherokee, Collingsworth, Comanche, Concho, Cooke, Crane, Dallas, Delta, Denton, Ector, El Paso, Falls, Fannin, Freestone, Goliad, Gray, Gregg, Grimes, Guadalupe, Hall, Hamilton, Hardin, Harris, Henderson, Hood, Hopkins, Howard, Hutchinson, Jefferson, Jim Wells, Karnes, Kaufman, Lavaca, Limestone, Lubbock, Madison, Matagorda, Maverick, McLennan, Medina, Midland, Moore, Nacogdoches, Navarro, Orange, Palo Pinto, Parker, Potter, Randall, Red River, Refugio, Robertson, Runnels, San Saba, Shelby, Smith, Somervell, Tarrant, Titus, Trinity, Tyler, Upshur, Uvalde, Val Verde, Victoria, Wichita, Wise, and Young.
Page Last Updated: 1/2/2024